A 60y old female pt came with c/o fever ,vomiting and headache since 4 days
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent.
Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs.
This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment box is welcome.
CASE PRESENTATION:
A 60y old female patient came to opd with c/o
1.fever since 4 days
2.C/o headache since 4 days
3.vomitings since 4 days
Patient was apparently asyptomatic 4 days back ,
later she had fever which was insidious in onset,progressive,low grade and not a/w chills,intermittent type with no diurnal variations,no aggregating or relieving factors
C/o headache since 4 days ,diffuse type not a/w diplopia,blurring of vision.No h/o any head trauma
C/o body pains since 4 days (generalized)
C/o vomiting since 4 days 2-3 episodes of vomitings with contents of food particles,non foul smelling,non bilious,non projectile .No h/o pain abdomen
H/o loose stools since 1 day (1 episode).non blood stained
No h/o cold ,cough,headache,burning micturition,haematuria,sob,chest pain,pedal edema
PAST HISTORY: k/c/o Thyroid since 8 years (on tab.carbimazole 10mg)
Not k/c/o DM,HTN,asthma,CKD,CHD
Non alcoholic and non smoker.No other addictions
HABITS: He was on mixed diet, appetite normal, constipation only on high protein diet
GENERAL EXAMINATION: pt is conscious, coherent, cooperative and oriented to time, place and person
No pallor,Icterus,cyanosis,clubbing, lymphadenopathy,edema
VITALS:
Temp:99.1f on presentation
BP:70/40mmhg on presentation
PULSE:79pm
RR:21cpm
Spo2:98% on RA
GRBS:124mg/dl
PER ABDOMEN:
Soft,non tender
Bowel sounds +
CVS:s1 s2 heard, no murmurs
RS: BAE clear, normal vesicular breath sounds heard,no added sounds
CNS: higher mental functions: normal
Cranial nerves: intact
Motor system: intact
Sensory system: intact
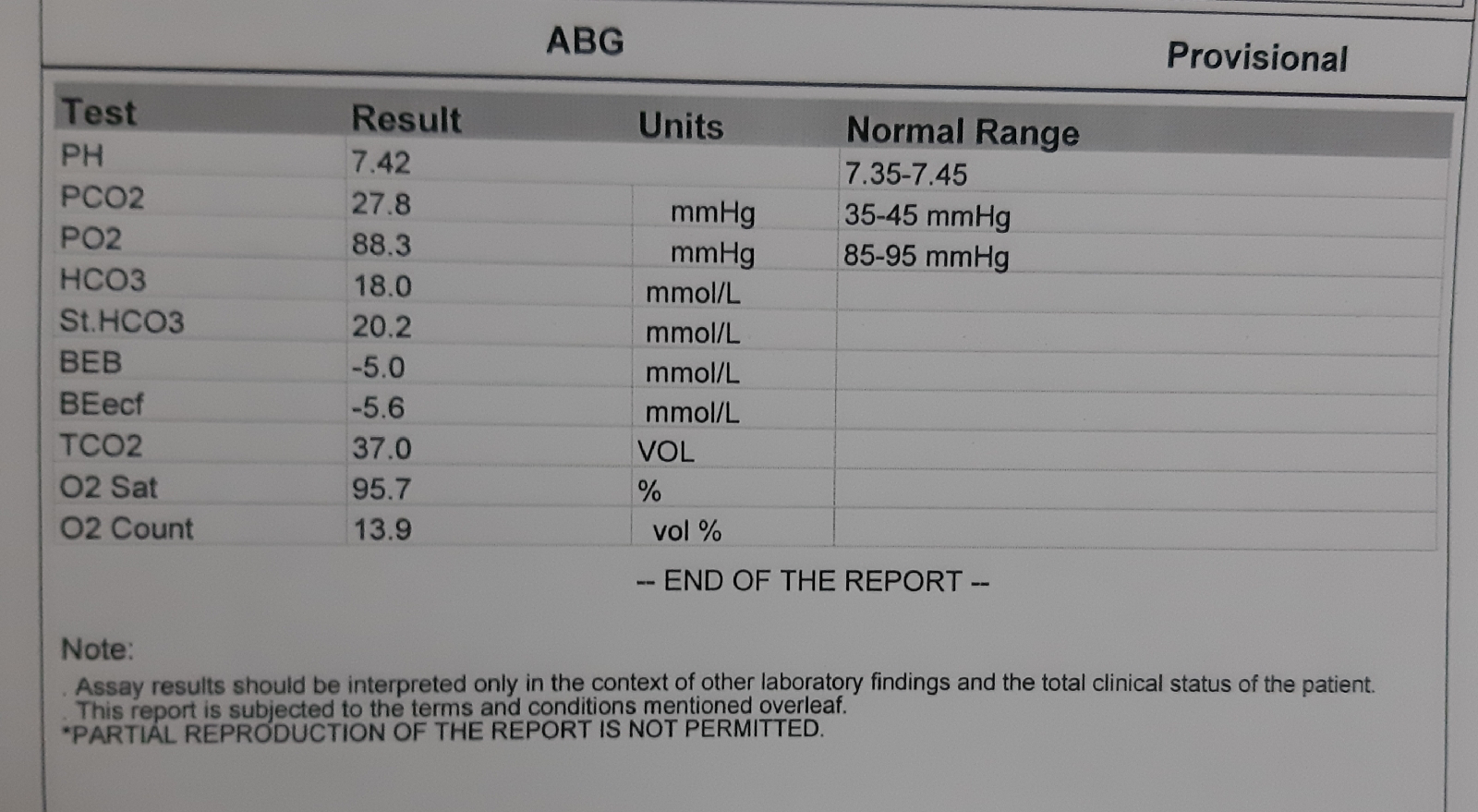
INVESTIGATIONS:









Comments
Post a Comment